By Chris Garvey, Rebecca Crouch, David Verrill
Field Tests (Walking Tests)
Field (walking) tests are commonly used for measurement of functional capacity in the pulmonary rehabilitation setting. Advantages include that the tests are functional, generally safe and easy to perform, inexpensive, and do not require extensive or expensive equipment. These tests are easily administered in the majority of pulmonary rehabilitation patients, including those that are debilitated. However, the test does not offer comprehensive physiological monitoring.
Six-Minute Walk Test
The 6-minute walk test (6MWT) is a widely used outcome measure for pulmonary rehabilitation. The test is safe, easy to administer, involves the use of minimal technical resources, is well tolerated, and accurately reflects a familiar activity of daily living (walking). The 6MWT measures the maximum distance walked in 6 minutes. To obtain valid and reliable results, it is essential to standardize the test procedure, such as staff, configuration of track, patient instructions and verbal reinforcement during testing, type, use and flow rate of supplemental oxygen, and walking aids.
One must consider the energy expenditure changes that occur while performing the 6MWT under certain circumstances, such as while using an assistive walking aid (e.g., rollator) and when a supplemental oxygen source is placed on the walking aid. It has been suggested that there are a reduction of breathlessness and an improvement in the distance walked when using a walking aid or supplemental oxygen. One study found as much as a 20 to 25% energy cost savings with the addition of a walking aid that supported supplemental oxygen. These energy savings appear to be most notable in persons with COPD who have lower exercise performance; e.g., 6MWT distance of
Directions on performing the 6MWT are given below.
Before the Test
- Standardize the shape of the flat walking course: straight versus continuous circle, oval, or square. If using a corridor, a minimum of 30 meters (98.4 feet) that is free of traffic and obstacles should be used.
- A comfortable ambient temperature and humidity should be maintained for all tests.
- A medical history for the patient has been reviewed and any precautions or contraindications to exercise testing have been taken into account (see absolute and relative contraindications, figures 3.4 and 3.5 later in the chapter).
- Instruct the patient to dress comfortably, wear appropriate footwear, and avoid eating or drinking for at least 2 hours before the test (when possible or appropriate).
- Prescribed inhaled bronchodilator medications should be taken if ordered within 1 hour of testing or when the patient arrives for testing.
- Rest for at least 10 minutes before beginning the test. If two tests are performed on the same day, at least 30 minutes rest should be allowed between tests.
- Record blood pressure BP, HR, SpO2, and dyspnea score while the patient is sitting or standing. Measure HR and SpO2 continuously during the test.
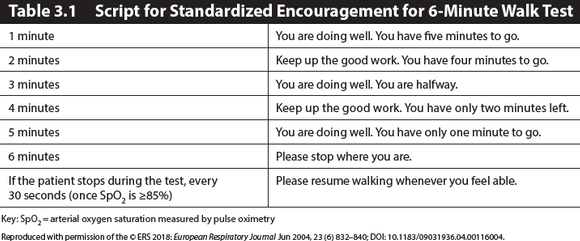
- Describe the walking track to the patient and give the patient standardized instructions (see table 3.1).
- If the patient has not performed a 6MWT in the recent past, two tests should be performed for initial testing due to a significant learning effect. Use the greater of the two test results.
During the Test
The patient should be asked to walk as far as he or she can in 6 minutes. Standardized encouragement and notification of time elapsed should be given at specific intervals according to the European Respiratory Society (ERS)/American Thoracic Society (ATS) 6MWT script (see table 3.1). Rests are allowed and included in the total test time. If the patient stops during the test (once SpO2 is ≥85%), advise the patient every 30 seconds to “please resume walking whenever you feel able”.
- The total distance covered is recorded.
- The patient is asked to rate shortness of breath and effort using a validated dyspnea and fatigue scale.
- The patient should walk alone; staff, other patients, or family should not walk with the patient performing the test. If necessary to have staff close to the patient during the walk for safety, they should walk behind the patient.
- Oxygen flow should be held constant during any test; oxygen titration should not be performed during a measured distance outcome walk test. Subsequent tests should use the same flow rate and modality if possible and safe.
- Staff should not assist the patient in carrying or pulling supplemental oxygen unless the patient cannot safely maneuver oxygen.
- Count laps with a lap counter.
- The patient may use their usual ambulatory assistive device; make note of which device (e.g., single-point cane, rollator walker, standard walker) is used and why.
- Monitor the patient for untoward signs and symptoms, including continuous SpO2 and HR.
- The oximeter should not be held by the patient. Either a finger oximeter or a handheld oximeter in a pouch should be used.
Ending the Test
- Once the 6 minutes are completed, the patient is instructed to stop where he or she is.
- Note if the patient exhibits any untoward signs and symptoms.
- Stop the test for:
- SpO2 desaturation <80%
- Chest pain
- Intolerable dyspnea
- Intolerable leg cramps, signs of intolerance to exercise exertion such as staggering, or unusual diaphoresis
- Pale or ashen appearance
- Immediately record SpO2, HR, dyspnea, fatigue, and blood pressure while patient is sitting (measurements taken before and after the test should be done with the patient in the same position).
- Record the distance completed in feet or meters, number of rest stops, total time of stops, and final vital signs including the lowest SpO2 level (and oxygen flow rate if used) on a standardized recording form.
Figure 3.2 shows a sample evaluation form for use in the 6MWT. The MET level corresponding to the average walking speed can be estimated based on the distance walked in 6 minutes. One MET is the amount of energy required while the body is at rest. This may be useful information for assessing exercise capacity and formulating an initial exercise prescription (see figure 3.3). Other information can be gleaned from the test, including gait analysis, balance, fatigue, and pain assessment.
The 6MWT can be influenced by multiple factors, including motivation, encouragement, learning effect, physical course layout, testing environment, gender, and age. Standardized encouragement must be given. There is a learning effect in performing successive 6MWTs, and distances may increase by 26.3 meters on subsequent tests; therefore, two walks should be performed during the initial testing, using the furthest distance of the two tests. If two tests are performed, the recommendation is to wait at least 30 minutes, or up to the next day, to repeat the second test and that the greater of the two values be reported.
The use of a treadmill for 6MWT is not advised. The physical layout of the course may impact walking distance. In the National Emphysema Treatment Trial (NETT), centers that used continuous walking courses, either oval or square, reported longer 6MWT distances than those with straight courses. The difference attributable to the course layout was 110 feet (33.5 meters), or a 10% advantage for continuous courses. The difference between straight and continuous courses may be due to the time and effort required for the subject to turn around on a straight course. The preassessments and postassessments in pulmonary rehabilitation, therefore, must use the same course to eliminate this potential variability.
Prediction formulas for the 6MWT distance are available. This information can be used to assess the patient’s level of impairment, compared to data from healthy adults. If using a prediction formula, the formula should be derived populations similar to the pulmonary rehabilitation program population. The minimal clinically meaningful change or minimum clinically important difference (MCID) in the 6MWT distance has been reported to be a mean of 30 meters (98.4 feet). For those patients who walk a very short distance in their initial 6MWT (
Shuttle Walk Tests
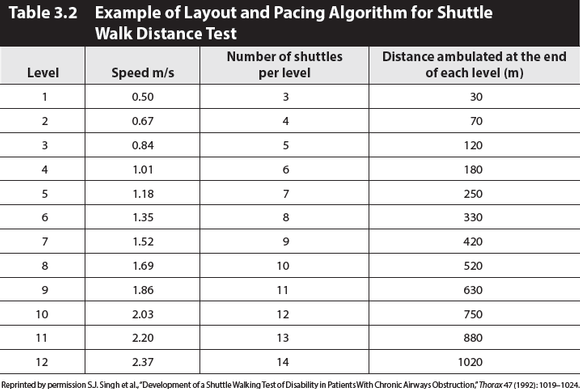
There are two types of shuttle walk tests: the incremental and the endurance shuttle walk tests. The ISWT is an incremental, symptom-limited walk test that simulates a symptom-limited cardiopulmonary exercise test (CPET). It measures a symptom-limited walking distance over a marked walking course of 10 meters (33 feet). This distance correlates well with maximal oxygen uptake. The ISWT utilizes an audible pacing timer to incrementally increase the pacing frequency (table 3.2). The subject walks according to the pacing timer frequency until they are too breathless to continue or cannot keep pace with the external pacing signal. Like the 6MWT, the primary test result of the ISWT is the total distance walked. As with the 6MWT, the ISWT should be performed twice prior to an intervention, with the best result recorded. The patient should rest for 30 minutes between tests. Directions for performing the ISWT are given below.
The endurance shuttle test (ESWT) is a standardized, externally controlled, constant-paced walking test for the assessment of endurance capacity. The ISWT is initially performed to determine exercise capacity, and then a paced walk speed corresponding to 85% of walking speed on the ISWT is used to determine the walking speed for the ESWT. The ESWT is a field test equivalent of the constant workload test. The primary outcome of the ISWT is distance, measured to the nearest 10 meters, whereas the primary outcome of the ESWT is time, consistent with other endurance tests.
Since exercise endurance improves more than peak oxygen concentration (peak (O2) after pulmonary rehabilitation exercise training, the ESWT is more responsive to pulmonary rehabilitation than the ISWT. For the ISWT, a change of distance of 47.5 meters has been described as associated with feeling “slightly better,” while a change of 78.7 meters has been associated with feeling “better”; therefore, the MCID for the ISWT distance in COPD is 47.5 meters. Preliminary data suggests the MID for the ESWT is in the region of 180 seconds.
Before the Test
- A medical history for the patient has been reviewed and any precautions or contraindications to exercise testing have been taken into account.
- Instruct the patient to dress comfortably, wear appropriate footwear, and avoid eating or drinking for at least 2 hours before the test (when possible or appropriate).
- Prescribed inhaled bronchodilator medications should be taken if ordered within 1 hour of testing or when the patient arrives for testing.
- Two cones are set 9 meters apart. The distance walked around the cones is 10 meters.
- The patient should rest for at least 15 minutes before beginning the test.
- Record blood pressure, HR, SpO2, and dyspnea score while the patient is sitting or standing.
During the Test
- Standardized instructions should be used via an audio recording.
- No encouragement should be given throughout the test.
- Record each shuttle that is completed on the recording sheet.
- The subject is asked to rate dyspnea and effort using a validated scale.
- The patient should walk alone; staff, other patients, or family should not walk with the patient performing the test.
- Do not assist the patient in carrying or pulling his/her supplemental oxygen.
- The patient may use an ambulatory assistive device; make note of which device (e.g., single-point cane, rollator, standard walker) is used and why.
- A comfortable ambient temperature and humidity should be maintained for all tests.
- Monitor the patient for untoward signs and symptoms.
- Stop the test for:
- Chest pain suspicious of angina.
- Evolving mental confusion or lack of coordination.
- Evolving light-headedness.
- Intolerable dyspnea.
- Leg cramps or extreme leg muscle fatigue.
- Persistent SpO2 ″ 85%.
- Any other clinically warranted reason.
Ending the Test
- The patient is more than 0.5 meter (1.6 feet) away from the cone when the beep sounds (allow one lap to catch up).
- The patient determines that he or she is too breathless to continue.
- For the endurance shuttle walk test (ESWT): The patient reaches 85% of predicted maximum HR.
- The patient exhibits any untoward signs and symptoms.
- Immediately record SpO2, HR, and dyspnea rating while the patient is sitting or standing (measurements taken before and after the test should be done with the patient in the same position).
- Two minutes later, record SpO2 and HR to assess the recovery rate.
- Record the total number of shuttles completed.
- Record the reason for terminating the test.
Adapted from C. Garvey, AACVPR Pulmonary Rehabilitation Outcome Toolkit, https://www.aacvpr.org/Member-Center/Pulmonary-Rehab-Outcomes-Resource-Guide 2017.
Proponents argue that, when compared to a self-paced 6MWT, the shuttle tests are less influenced by motivation or pacing, correlate better with exercise capacity in patients with chronic lung disease, and may be a more sensitive indicator of functional change with rehabilitation or other therapies. Performance on the ISWT relates strongly to direct measures of peak (O2, allowing the prediction of peak (O2. During the ISWT, the cardiorespiratory response to exercise (peak (O2) develops in an incremental fashion similar to formal CPET, thus making this a simple test requiring less technical expertise and equipment. Furthermore, the ISWT is easier to administer, is less expensive, and incorporates an activity that patients perform on a daily basis (i.e., walking).