Misconceptions abound about our breathing, or ventilation (VE). Of course, ventilation is necessary for the exchange of gases between the atmosphere and our metabolism. We use oxygen (O2) from the atmosphere as the final electron acceptor in the electron transport chain. We must also expire carbon dioxide (CO2), since this carbon is the result of macronutrient combustion (refer to lab 5). During exercise, O2 consumption and CO2production increase; therefore, we need to increase our ventilation. As you learned in labs 9 and 10, we ventilate much more at higher workloads above the ventilatory threshold. This is the result of greater CO2production at higher intensities from the buffering of lactate (see labs 9 and 10), or in other words, respiratory compensation for metabolic acidosis. Thus our lungs act to regulate acid-base balance.
At normal altitudes, our ventilation is more sensitive to the production of CO2 than it is to the consumption of O2. Very small increases in PCO2 results in a proportional increase in V.E, whereas PO2 can decrease significantly with little effect on the stimulation of VE(see figure 13.1, a and b). At high altitudes (> 2,000 m or 6,500 ft), the reduced partial pressure of O2 (which can lead to hypoxia) is capable of stimulating greater amounts of ventilation. Not only do changes in CO2 and O2stimulate us to breathe differently; we also have voluntary control over our breathing.
The increased need for ventilation during exercise as the result of increased CO2 production and O2consumption leads us as exercise physiologists to be interested in its measurement. We move atmospheric gases into our lungs by creating negative pressures in our thoracic cavity.

This is accomplished by the skeletal muscles of inspiration (diaphragm, intercostals) and expiration (intercostals, abdominals), which change the volume within the thoracic cavity—the greater the change in volume, the bigger our breath, or tidal volume (VT). Ventilation is, therefore, a function of breathing frequency (bf) multiplied by tidal volume (VT):
VE(L · min-1) = bf (b · min-1) X VT(L · b-1)
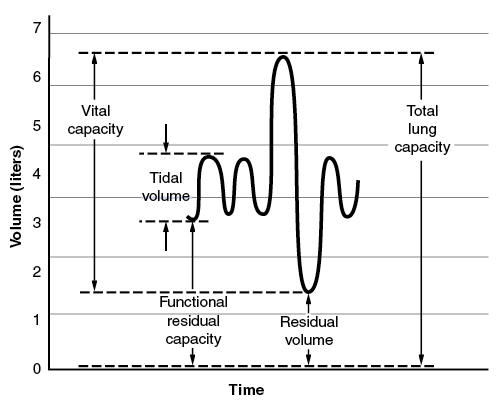
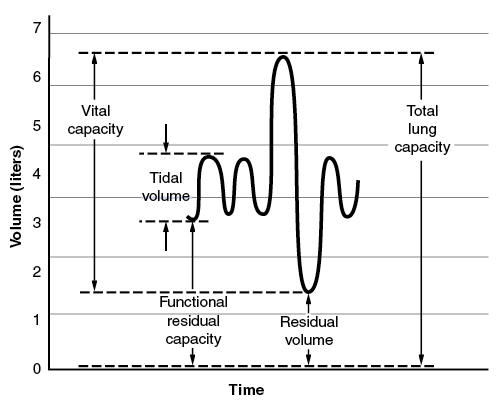
Tidal volume is one of the measurements made during spirometry. Ventilation can be divided into distinct volumes and capacities, as seen in figure 13.2.
Pulmonary Function Testing
A pulmonary function test (PFT) can measure the amount (volume) and speed (flow rate) of inspiration and expiration. PFTs can be used to identify the health and capacity of the pulmonary system. Most PFTs can measure tidal volume (VT), as well as the following:
- forced vital capacity (FVC)—Maximum volume forcibly expired after maximum inspiration (in liters).
- forced expiratory volume (FEV1.0)—Volume of air exhaled in the first second after maximal inhalation; used as a diagnostic tool for limitations in flow rates (expressed in liters but by the definition L · s-1).
- FEV1.0/FVC ratio—Ratio of FEV1.0 to FVC, which is a common measure of pulmonary disease (see later in this chapter); in healthy individuals, about 70% to 85% (ratio reduced in COPD patients but may be normal in restrictive diseases).
- peak expiratory flow (PEF)—Maximum expiratory flow during a forced expiration from the point of maximum inspiration (total lung capacity); expressed in L · min-1or L · s-1 and used to provide a measure of airway caliber (diameter) and airflow (yet is dependent not only on airway caliber but also on lung elastic recoil, patient effort, and patient cooperation); generally less specific than FEV1.0 as a diagnostic measure.
- maximum voluntary ventilation (MVV)—Maximal amount of air expired in one minute (L · min-1).
- maximum exercise ventilation (VEmax)—Maximal volume expired during maximal exercise (L · min-1).
- residual volume (RV)—Amount of air remaining in the lungs following a maximal expiration (in liters).
- total lung capacity (TLC)—Vital capacity and residual volume combined for the total volume of the lungs (in liters).
Lung volumes are largely a function of age, height, and sex. Physical fitness does not significantly affect lung size per se, but it may improve measurement of flow rates, though this idea may be challenged by some evidence concerning swimmers (4, 22).
Volumes for PFT results are usually expressed in terms of BTPS (body temperature and pressure, saturated). You may recall that volumes of gases are dependent on the temperature, barometric pressure, and level of humidity, or water saturation. As a result, expression of gas volumes needs to have a systematic unit of expression. Since the air in our lungs is at body temperature, ambient pressure, and nearly 100% humidity, the units of BTPS are common for PFT results. However, as you exhale air and it cools to the temperature of the room and loses humidity or condenses, its volume changes. Thus, it may be necessary to convert from ambient (or room) temperature, ambient pressure, saturated (ATPS). Your laboratory instructor can indicate whether this is necessary. The equation for converting ATPS to BTPS is as follows (where VATPS = volume of gas at ATPS, TA= temperature in your lab, PB= barometric pressure in your lab, and PH2O= water vapor pressure at the TA):
VBTPS = VATPS X [310 / (273 + TA)] X [(PB - PH2O) / (PB - 47)]
PFT as a Tool for Diagnosing Pulmonary Disease
PFT results can be used in diagnoses of respiratory diseases, which are categorized into two different types (based on PFT results): obstructive and restrictive.
An obstructive diseaseis characterized by an acute or chronic obstruction in the bronchi leading to the alveoli. These obstructions are often referred to as chronic obstructive pulmonary diseases (COPDs). Individuals with these diseases usually have normal lung volumes but restricted flow rates. COPDs can be diagnosed by testing the FEV1.0, FEV1.0/FVC ratio, PEF, or other flow rate measures. Examples of COPDs include asthma, chronic bronchitis, and emphysema. Asthma differs from the other two in that it can be temporary and reversible. Exercise-induced asthma is a temporary inflammatory response during exercise that obstructs ventilatory flow rates. Exercise-induced asthmatics may have normal flow rates at rest but produce a positive test (i.e., a 15% decrease from pre-exercise measured FEV1.0) following 6 to 8 min of vigorous exercise at a target intensity of 85% to 90% of maximum heart rate.
A restrictive disease is characterized by reduced total lung capacities or volumes, such as TLC or vital capacity (VC), but the individual may have normal flow rates. Restrictive diseases can be diagnosed by measuring FVC or a slow VC. Examples of restrictive diseases include pulmonary fibrosis, scar tissue, and tumors.
Pulmonary Disease Classifications
For both obstructive and restrictive pulmonary diseases, PFT results are classified by the following comparisons with predicted results (for restrictive diseases, FVC is comparison; for COPDs, % predicted is for FEV1.0) (23):
Good: >100% of predicted
Normal: 100% to 80% of predicted
Mild: 80% to 65% of predicted
Moderate: 65% to 50% of predicted
Moderately severe: 50% to 35% of predicted
Severe:
Individuals with pulmonary disease have increased work of breathing and, if severe enough, limited O2 delivery to working tissues, including the brain. Under these circumstances, exercise is extremely uncomfortable, and supplemental oxygen may be necessary for activities of daily living. Despite the discomfort of exercise for these individuals, it can alleviate many of their symptoms. For further information on pulmonary rehabilitation, refer to reference sources 10, 11, 27, as well as the following sources from Human Kinetics: 1, 3, 18, 19.
Selected References
1. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Pulmonary Rehabilitation Programs. 4th ed. Champaign, IL: Human Kinetics, 2011.
3. Babcock MA, Pegelow DF, Harms CA, and Dempsey JA. Effects of Respiratory Muscle Unloading on Exercise-Induced Diaphragm Fatigue. J Appl Physiol 93: 201–206, 2002.
4. Black LF, Offord K, and Hyatt RE. Variability in the Maximal Expiratory Flow Volume Curve in Asymptomatic Smokers and in Nonsmokers. Am Rev Respir Dis 110: 282–292, 1974.
10. Ferreira SA, Guimaraes M, and Taveira N. Pulmonary Rehabilitation in COPD: From Exercise Training to “Real Life.” J Bras Pneumol 35: 1112–1115, 2009.
11. Ghanem M, Elaal EA, Mehany M, and Tolba K. Home-Based Pulmonary Rehabilitation Program: Effect on Exercise Tolerance and Quality of Life in Chronic Obstructive Pulmonary Disease Patients. Ann Thorac Med 5: 18–25, 2010.
18. Jobin J, Maltais F, LeBlanc P, and Simard C. Advances in Cardiopulmonary Rehabilitation. Champaign, IL: Human Kinetics, 2000.
19. Jobin J, Maltais F, Poirier P, LeBlanc PJ, and Simard C. Advancing the Frontiers of Cardiopulmonary Rehabilitation. Champaign, IL: Human Kinetics, 2002.
22. Mickleborough TD, Stager JM, Chatham K, Lindley MR, and Ionescu AA. Pulmonary Adaptations to Swim and Inspiratory Muscle Training. Eur J Appl Physiol 103: 635–646, 2008.